Nutritional Strategies for Managing NAFLD:
A Genomic Approach

Non-Alcoholic Fatty Liver Disease (NAFLD) has evolved into a global health crisis, affecting millions worldwide. In India, this metabolic disorder is of particular concern due to shifting dietary habits and sedentary lifestyles, contributing to its increasing prevalence. While traditional risk factors like diet and lifestyle have long been associated with NAFLD, recent advances in nutrigenomics have highlighted the significance of genetic predisposition in the development and progression of this condition. In this comprehensive blog, we will explore the multifaceted aspects of NAFLD, from global and Indian statistics to the role of genetics, nutrigenomics, and nutrient interventions, offering practical guidance for managing NAFLD effectively.
Understanding NAFLD: A Multifactorial Condition
NAFLD encompasses a range of liver disorders characterised by the build-up of fat in liver cells, in the absence of excessive alcohol consumption. The complex interplay of multiple factors, including genetics, insulin resistance, oxidative stress, inflammation, and lifestyle choices, contributes to the development and progression of NAFLD. The disease is progressive and has grades.
1. Grade 1 (Steatosis): In this initial stage, also known as Steatosis, individuals experience the accumulation of fat in liver cells, often without significant inflammation or liver damage.
2. Grade 2 (NASH - Non-Alcoholic Steatohepatitis): NASH represents a more advanced stage where not only fat but also inflammation and liver cell damage are present, increasing the risk of complications.
3. Grade 3 (Fibrosis): Fibrosis indicates the development of scarring or fibrous tissue in the liver, signifying a progression towards more severe liver damage.
4. Grade 4 (Cirrhosis): The most severe stage, Cirrhosis, signifies extensive scarring and liver dysfunction, often leading to significant health complications and liver failure.
Genetics and NAFLD Risk
Recent scientific findings suggest that genetic factors significantly influence an individual's susceptibility to NAFLD. Various genes and genetic variants have been identified as key players in NAFLD, impacting lipid metabolism, insulin sensitivity, inflammation, and fibrosis.
One such variant is found in the PNPLA3 gene, which is strongly associated with increased hepatic fat accumulation and a heightened risk of NAFLD. Other genes like TM6SF2, GCKR, and MBOAT7 have also been linked to disease progression and fibrosis.
Nutrigenomics: A Personalised Approach
Nutrigenomics, a cutting-edge field, explores how an individual's genetic makeup shapes their response to nutrients and dietary components. This approach starts with a comprehensive genetic analysis to identify susceptibility genes and variants.
Genetic Risk Assessment
Genetic profiling plays a pivotal role in recognizing specific genes and variants linked to NAFLD susceptibility. For example, assessing variants in PNPLA3, TM6SF2, GCKR, and MBOAT7 helps gauge an individual's genetic risk (Krawczyk et al., 2014).
Personalised Dietary Recommendations
Once genetic variants are identified, personalised dietary recommendations can be tailored to mitigate an individual's genetic predispositions. For instance, individuals with the PNPLA3 variant may benefit from a diet low in saturated fats and rich in unsaturated fats, as indicated by studies (Romeo et al., 2008; Dongiovanni et al., 2015).
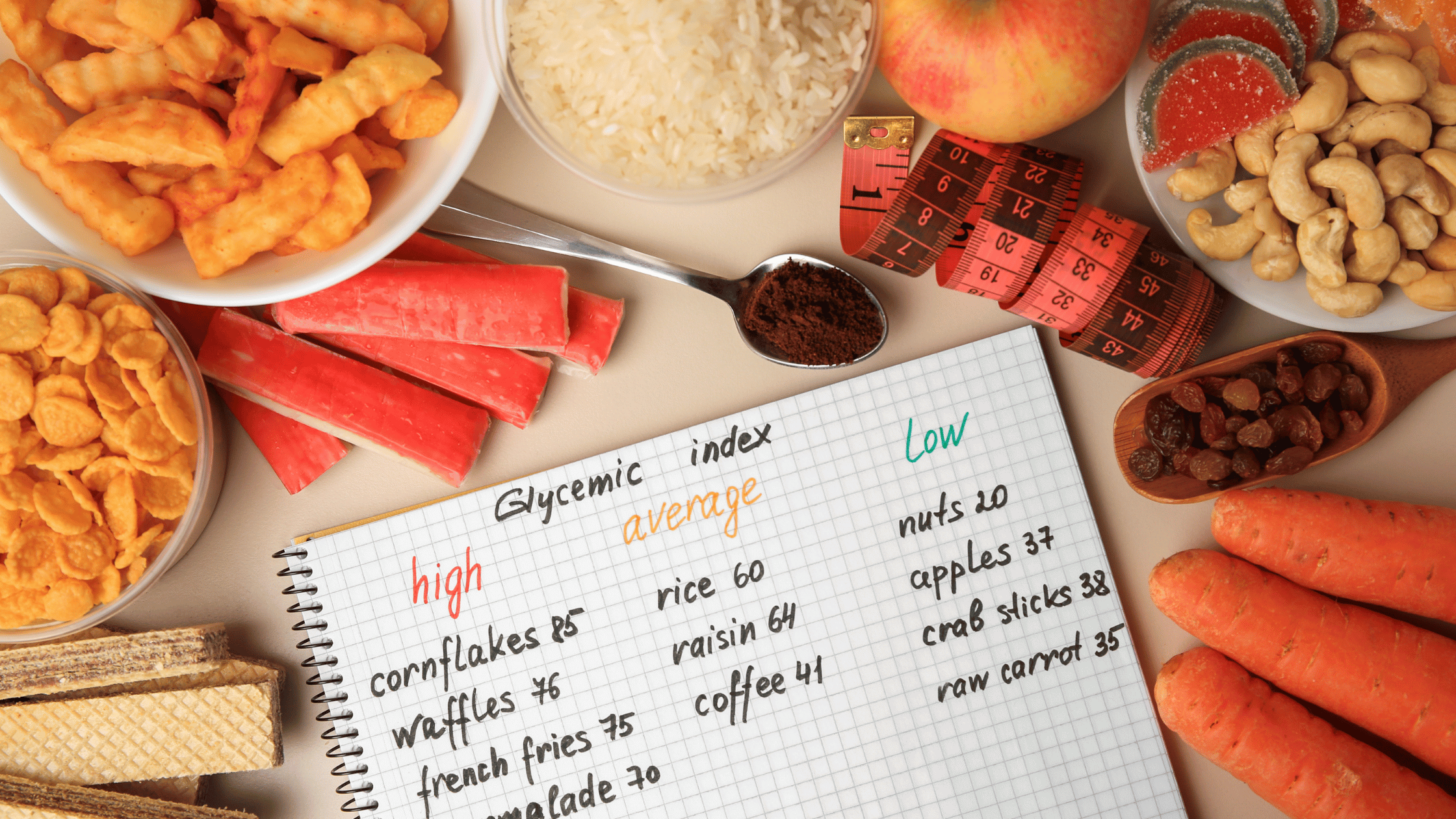
Nutrients and Metabolites
Nutrigenomics also focuses on specific nutrients and metabolites that can impact NAFLD. Nutrients such as omega-3 fatty acids, vitamin D, and antioxidants have demonstrated promise in reducing liver fat and inflammation. Monitoring key metabolites, including serum triglycerides, adiponectin, and hepatic enzymes, can help assess disease progression and response to dietary interventions.
For example, omega-3 fatty acids, prevalent in fatty fish like salmon, have been linked to improved liver fat content reduction and reduced inflammation (Ryan et al., 2014). Vitamin D supplementation has shown potential in addressing insulin resistance and reducing liver fat accumulation (Eslam et al., 2017).
Global and Indian NAFLD Statistics
NAFLD's global prevalence is alarming, affecting about 25% of the global population. In India, rapid urbanisation and lifestyle changes have led to an estimated 9-32% prevalence of NAFLD, making it a significant public health concern.
Here's a table summarising possible nutrient interventions for different grades of NAFLD: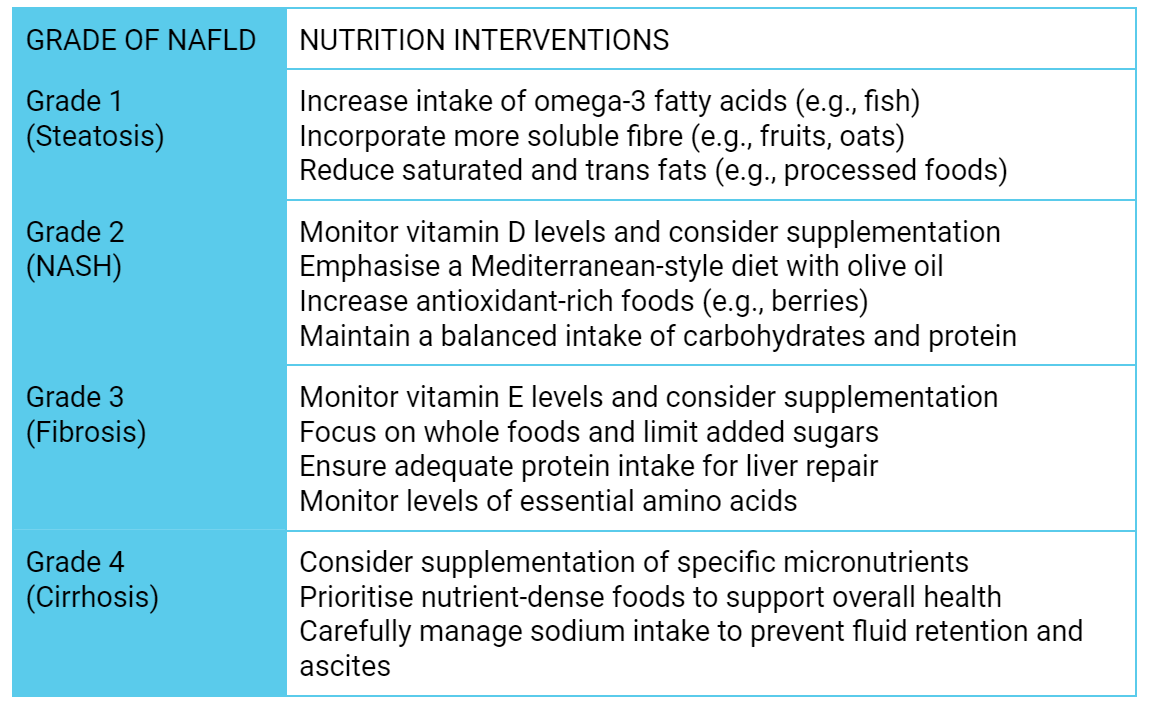
In conclusion, NAFLD is a multifaceted condition influenced by genetic and environmental factors. Nutrigenomics offers an exciting avenue for personalised NAFLD management, tailoring dietary and lifestyle recommendations to an individual's unique genetic profile. In addition to genetic assessments, specific nutrients and metabolites can be harnessed as key tools in the battle against NAFLD. While nutrigenomics holds immense promise, it should be integrated with traditional medical guidance to provide a comprehensive approach to NAFLD prevention and treatment. As our understanding of nutrigenomics deepens, we anticipate more refined and effective strategies for managing NAFLD, both globally and in countries like India, where the burden of the disease continues to grow.
References:
1. Romeo, S., Kozlitina, J., Xing, C., et al. (2008). Genetic variation in PNPLA3 confers susceptibility to nonalcoholic fatty liver disease. Nature Genetics, 40(12), 1461-1465.
2. Dongiovanni, P., Petta, S., Maglio, C., et al. (2015). Transmembrane 6 superfamily member 2 gene variant disentangles nonalcoholic steatohepatitis from cardiovascular disease. Hepatology, 61(2), 506-514.
3. Ryan, M. C., Itsiopoulos, C., Thodis, T., Ward, G., Trost, N., Hofferberth, S., & O'Dea, K. (2014). The Mediterranean diet improves hepatic steatosis and insulin sensitivity in individuals with non-alcoholic fatty liver disease. Journal of Hepatology, 59(1), 138-143.
4. Eslam, M., George, J., & Qiao, L. (2017). Vitamin D: A role in hepatology? The Journal of Hepatology, 67(5), 1013-1025.
5.Krawczyk, M., Liebe, R., Lammert, F., & Krawczyk, M. (2014). Genes in NAFLD: from susceptibility genes to therapeutic targets. Nature Reviews Gastroenterology & Hepatology, 11(6), 362-37

The Gene Box








.png)