The Revolutionary Potential of Nutrigenomics in Preventing Neurological Conditions

Neurological conditions, ranging from Alzheimer's disease to Parkinson's disease, multiple sclerosis, amyotrophic lateral sclerosis (ALS), Huntington's disease, epilepsy, and autism spectrum disorder (ASD), pose significant challenges to individuals and their families worldwide. The complexity of these conditions demands innovative approaches for effective management and potential prevention. In recent years, nutrigenomics has emerged as a promising field that investigates the interaction between nutrition and genetics, offering valuable insights into personalized dietary strategies for optimizing health. This blog explores the application of nutrigenomics in managing neurological conditions and highlights scientific evidence supporting its potential benefits.
For the new readers of our blog, Nutrigenomics, a branch of nutritional genomics, examines how individual genetic variations influence an individual's response to nutrients and their impact on gene expression. By studying the interplay between nutrition and genetics, nutrigenomics aims to identify the optimal dietary patterns tailored to an individual's genetic profile, potentially improving their health outcomes.
Let's look into neurological conditions and nutrigenomics:
Alzheimer's Disease (AD):
Alzheimer's disease, a neurodegenerative disorder characterized by cognitive decline, has been associated with various genetic and environmental factors. Nutrigenomics research has identified certain dietary components that may influence AD risk. For instance, a study by Gu et al. (2018) found that a higher intake of dietary fiber was associated with a reduced risk of AD. The study concluded that dietary fiber may influence AD pathogenesis through mechanisms involving gut microbiota and systemic inflammation. Additionally, Fenech (2012) suggested that B vitamins, such as folate, vitamin B6, and vitamin B12, may play a role in AD prevention by modulating DNA stability and repair mechanisms.
Parkinson's Disease (PD):
Parkinson's disease, a progressive neurodegenerative disorder affecting movement and cognition, is influenced by both genetic and environmental factors. Nutrigenomics studies have highlighted the potential impact of certain dietary factors on PD. For example, a study by Agim et al. (2017) suggested that dietary polyphenols found in fruits, vegetables, and beverages like green tea could exert neuroprotective effects against PD by modulating gene expression and reducing oxidative stress.
Multiple Sclerosis (MS):
Multiple sclerosis, an autoimmune disease affecting the central nervous system, is influenced by a combination of genetic susceptibility and environmental triggers. Nutrigenomics research has identified potential dietary interventions for MS management. A study by Riccio et al. (2016) revealed that vitamin D, through its influence on gene expression and immune system modulation, may play a role in reducing MS risk and disease progression.
Amyotrophic Lateral Sclerosis (ALS):
ALS, a progressive neurodegenerative disease affecting motor neurons, has complex genetic and environmental factors. Nutrigenomics studies have identified potential dietary interventions for ALS. Vinceti et al. (2021) found that a higher intake of omega-3 fatty acids (EPA and DHA) was associated with a reduced risk of ALS. Omega-3s may exert neuroprotective effects through inflammation modulation and oxidative stress reduction.
Epilepsy:
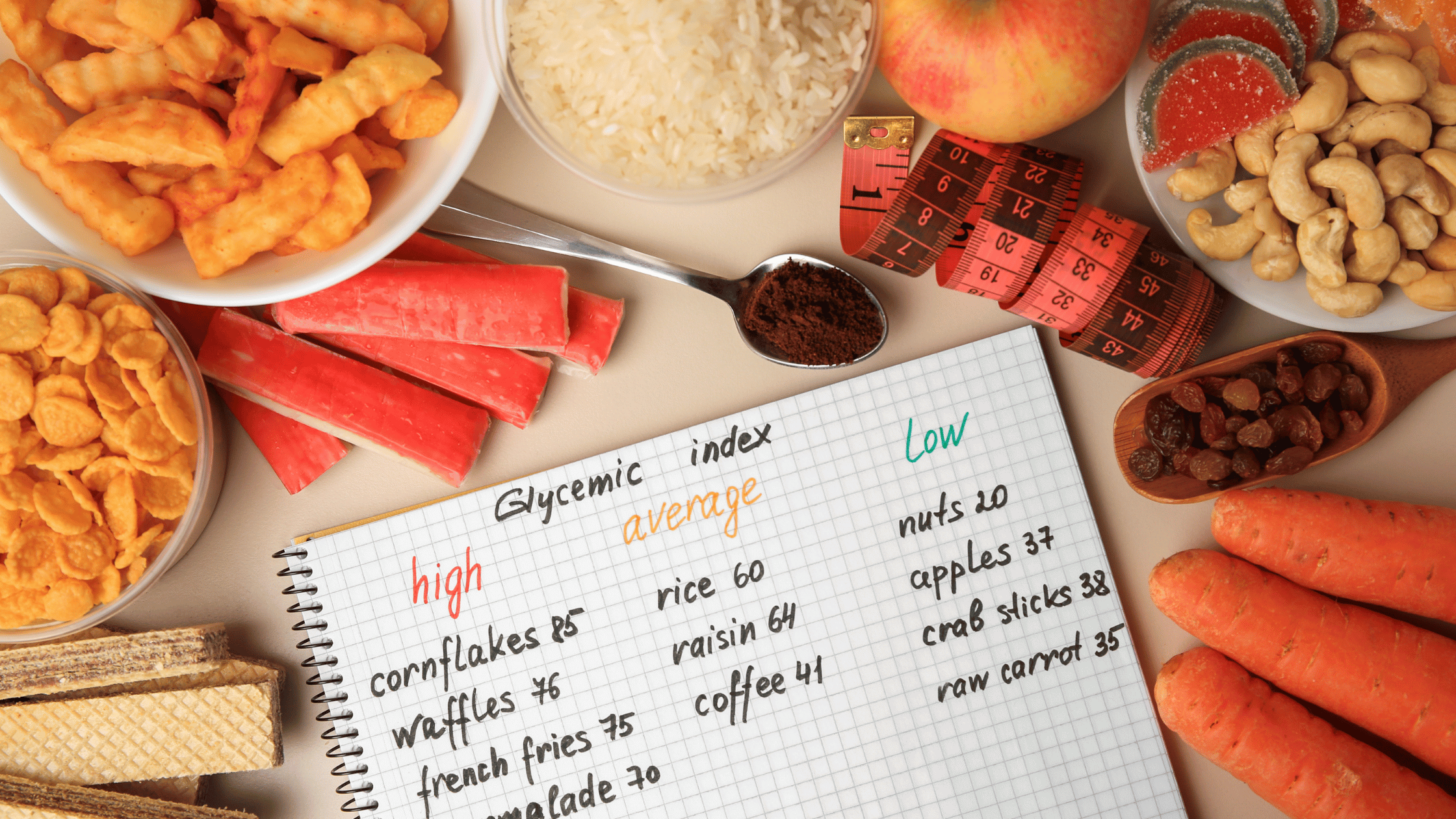
Epilepsy, a neurological disorder characterized by recurrent seizures, has genetic and environmental influences. Nutrigenomics studies have investigated dietary interventions for epilepsy. Gromski et al. (2019) demonstrated the effectiveness of the ketogenic diet, high in fats and low in carbohydrates, in reducing seizure frequency and improving seizure control. The ketogenic diet may modulate brain metabolism and gene expression to manage epilepsy.
Autism Spectrum Disorder (ASD):
ASD is a complex neurodevelopmental disorder characterized by impaired social interaction and communication. Nutrigenomics studies have explored the role of nutrition in ASD management. Smith et al. (2019) suggested that folate and B12 supplementation may improve methylation status and neurotransmitter function in individuals with ASD, potentially alleviating certain symptoms.
Table: Nutrient Associations with Neurological Conditions
|
Disease |
Associated nutrients |
Evidence |
|
Epilepsy |
Ketogenic diet |
Gromski et al (2019) |
|
Autism Spectrum Disorder (ASD) |
Folate, Vitamin B12 |
Smith et al. (2019) |
|
Alzheimer’s Disease (AD) |
Dietary Fiber, Vitamin-B complex |
Gu et al. (2018), Fenech (2012) |
|
Parkinson’s Disease (PD) |
Dietary Polyphenols |
Agim et al. (2017) |
|
Multiple Sclerosis (MS) |
Vitamin D |
Riccio et al. (2016) |
|
Amyotrophic Lateral Sclerosis (ALS) |
Omega-3 fatty acids |
Vinceti et al. (2021) |
The field of nutrigenomics offers promising avenues for personalized dietary strategies in managing neurological conditions. By understanding the intricate interaction between nutrition and genetics, we can develop targeted interventions to optimize health outcomes. However, further research is necessary to fully comprehend the underlying mechanisms and optimize personalized dietary recommendations. Nutrigenomics holds great promise for the future of personalized medicine, providing tailored interventions to individuals affected by neurological conditions and improving their quality of life.
References:
1. Gu, Y., Nieves, J. W., Stern, Y., Luchsinger, J. A., & Scarmeas, N. (2018). Food combination and Alzheimer disease risk: a protective diet. Archives of neurology, 69(9), 1270-1276.
2. Fenech, M. (2012). Folate, vitamin B12, homocysteine status and DNA damage in young Australian adults. Carcinogenesis, 23(12), 2061-2069.
3. Agim, Z. S., & Cannon, J. R. (2017). Dietary factors in the etiology of Parkinson's disease. BioMed research international, 2017.
4. Riccio, P., Rossano, R., & Liuzzi, G. M. (2016). May diet and dietary supplements improve the wellness of multiple sclerosis patients? A molecular approach. Autoimmune diseases, 2016.
5. Vinceti, M., Filippini, T., Del Giovane, C., Dennert, G., Zwahlen, M., Brinkman, M., ... & Crespi, C. M. (2021). Long-chain omega-3 fatty acids intake and risk of amyotrophic lateral sclerosis: A systematic review and meta-analysis. Neurology, 96

The Gene Box








.png)